IVF First Cycle Success Rate Calculator
Estimate Your First Cycle Success Rate
Based on data from over 150,000 IVF cycles (2022-2024)
Your Estimated Success Rate
Key Factors Affecting Your Odds
When you hear the term InVitroFertilization (IVF), the first question that pops up is usually, “Will it work for me right away?” The truth is a mix of statistics, age, health factors, and clinic quality. Below you’ll find a step‑by‑step breakdown of how successful a first IVF attempt really is, the numbers you can trust, and concrete actions you can take to boost your chances.
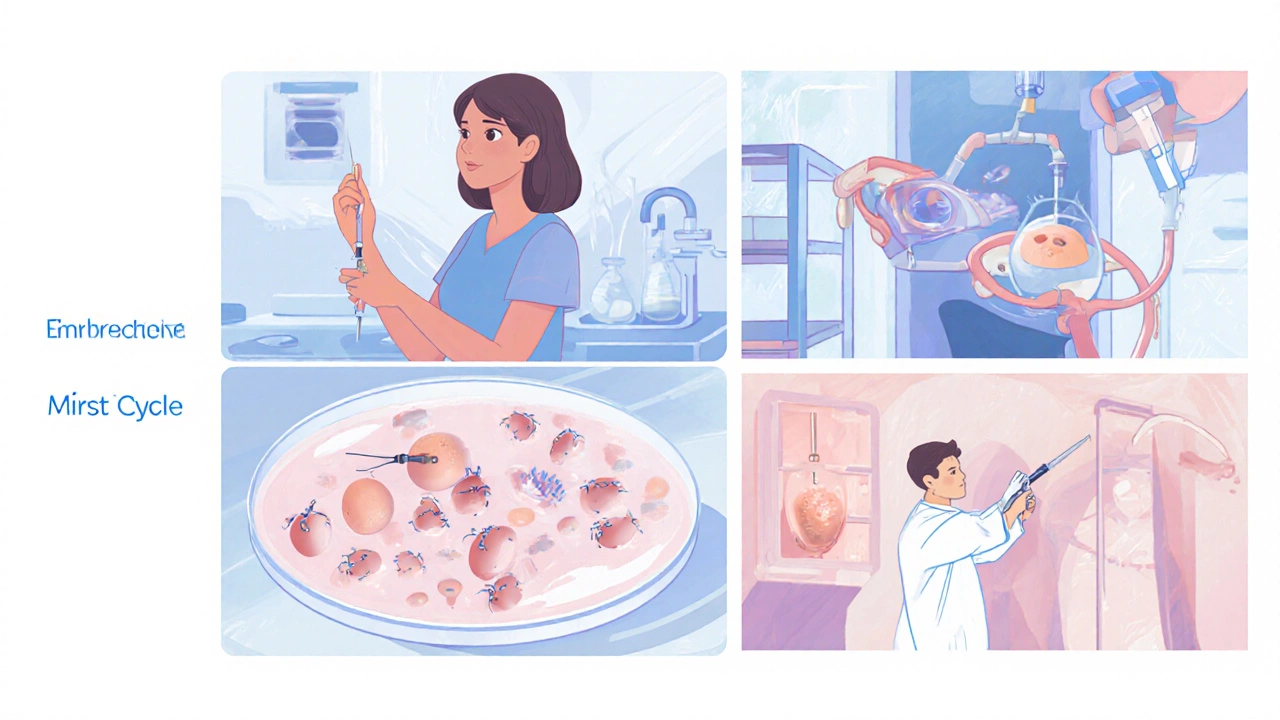
What Is IVF and How Does a First Cycle Work?
IVF is a fertility treatment where eggs are retrieved, fertilized with sperm in a lab, and the resulting embryo(s) are transferred back to the uterus. A typical first cycle involves four phases:
- Ovarian stimulation - hormones coax the ovaries to produce multiple eggs.
- Egg retrieval - a minor surgical procedure to collect the mature eggs.
- Laboratory fertilization - either conventional IVF or Intracytoplasmic Sperm Injection (ICSI) if sperm quality is a concern.
- Embryo transfer - usually one or two embryos are placed into the uterus.
The whole process spans roughly 4-6 weeks. Success hinges on how many high‑quality embryos survive to transfer and how receptive the uterus is at that moment.
Overall Success Rates for the First IVF Attempt
Globally, the average IVF success rate for a fresh, first‑cycle transfer hovers around 30% per started cycle, according to the 2024 International IVF Registry. That figure means roughly three out of ten couples achieve a clinical pregnancy the first time they try.
But “average” masks a lot of variation. Success is not a flat line; it bends dramatically with age, health metrics, and clinic experience. Below is a snapshot of pooled data from 2022‑2024 studies covering more than 150,000 cycles:
| Age Group | Live‑Birth Rate % | Clinical Pregnancy % |
|---|---|---|
| Under 35 | 42 | 50 |
| 35‑37 | 33 | 40 |
| 38‑40 | 25 | 30 |
| 41‑42 | 15 | 20 |
| 43‑44 | 8 | 12 |
| 45+ | 3 | 5 |
Notice the steep decline after 38years. Age is the single strongest predictor, outweighing even the most aggressive stimulation protocols.
Key Factors That Influence First‑Cycle Success
Beyond age, several measurable variables shift the odds. Each factor appears in research as an independent predictor when controlling for the others.
- Egg quality - closely tied to age and ovarian reserve (AMH levels). Higher quality yields more top‑grade embryos.
- Sperm quality - motility and morphology impact fertilization; ICSI can offset severe deficits.
- Embryo quality - assessed by morphology and, increasingly, by pre‑implantation genetic testing (PGT‑A).
- Body Mass Index (BMI) - a BMI between 18.5‑24.9 has the highest live‑birth odds; >30 can cut success by up to 15%.
- Uterine receptivity - optimal endometrial thickness (7‑9mm) and hormonal environment matter.
- Clinic experience - centers performing >200 cycles/year report roughly 5‑7% higher live‑birth rates.
Understanding where you stand on each of these helps you target the most impactful improvements before your first attempt.

Improving Your Odds Before the First Try
Here are evidence‑backed steps you can take in the three months leading up to stimulation.
- Optimize BMI. For overweight patients, a 5‑10% weight loss can raise live‑birth rates by 3‑5% according to a 2023 meta‑analysis.
- Quit smoking and limit alcohol. A 2022 cohort showed smokers had a 12% lower implantation rate.
- Screen for thyroid and vitamin D deficiencies. Correcting these has been linked to a 7% bump in pregnancy odds.
- Consider a pre‑IVF consultation with a reproductive endocrinologist to assess ovarian reserve (AMH, antral follicle count).
- If male factor is present, discuss ICSI early. Studies show ICSI can rescue fertilization in >90% of severe cases.
- Choose a clinic with transparent success data and a robust lab accreditation (e.g., CAP, ISO 15189).
These tweaks don’t guarantee a pregnancy, but they stack the odds in your favor without adding risk.
What Happens If the First Cycle Fails?
A failed cycle can feel crushing, but it also provides valuable data. Most clinics will review:
- Number and quality of retrieved eggs.
- Fertilization rate (how many eggs turned into embryos).
- Embryo grade and any genetic testing results.
- Endometrial thickness at transfer.
Armed with that information, you can adjust the protocol-perhaps increasing the stimulation dose, opting for a frozen‑thaw transfer, or adding PGT‑A to select the healthiest embryo. The cumulative live‑birth rate after two cycles climbs to about 55% for women under 35, according to the 2024 HFEA report.

Choosing the Right Clinic and Setting Realistic Expectations
Not all clinics report data the same way. Look for:
- Live‑birth rates per fresh embryo transfer (the most honest metric).
- Breakdown by age group-avoid clinics that only publish an overall “30%” figure.
- Accreditation and lab quality scores.
- Patient‑centered services (counseling, flexible scheduling).
When you have the numbers, set expectations that match your profile. For a 36‑year‑old with a normal BMI, a 30‑35% chance of pregnancy on the first try is realistic; expecting a 50% chance would be overly optimistic.
Quick Checklist Before Your First IVF Cycle
- Know your IVF success rate by age - use reputable registries.
- Get a baseline blood panel: AMH, FSH, thyroid, vitamin D.
- Calculate BMI and plan a healthy weight‑loss or gain strategy if needed.
- Discuss male factor and whether ICSI might be required.
- Choose a clinic with transparent age‑specific outcomes and accredited labs.
- Prepare mentally - consider counseling or support groups.
Frequently Asked Questions
What is the average live‑birth rate for a first IVF cycle?
Globally, the average live‑birth rate per first‑cycle fresh transfer is about 30%, but it rises to over 40% for women under 35 and drops below 10% after age 42.
Does using ICSI improve first‑cycle success?
ICSI mainly helps when sperm quality is low. It normalizes fertilization rates but doesn’t significantly change overall live‑birth odds unless male factor is the limiting issue.
Can pre‑implantation genetic testing (PGT‑A) raise my chances?
PGT‑A can increase live‑birth rates by 4‑6% in women under 38 by allowing the transfer of euploid embryos, but it adds cost and requires a freeze‑all approach.
How many cycles should I plan for?
Statistically, 50‑60% of couples achieve a live birth within three cycles. Many clinicians recommend budgeting for at least two attempts before reassessing strategy.
Is age the only factor I can’t control?
Age is the strongest predictor, but lifestyle, weight, and lab quality are modifiable. Optimizing those can offset some age‑related decline.