Herb Blood Pressure Estimator
Estimate Your Blood Pressure Change
Select an herb and enter your current systolic blood pressure to see potential effects.
Estimated systolic increase: 0 mmHg
Estimated new systolic BP: 0 mmHg
When it comes to natural remedies, many people assume herbs are always gentle. Licorice is a classic example of a plant that can actually push your systolic numbers higher if you’re not careful.
Why Some Herbs Spike Blood Pressure
Herbs contain bioactive compounds that interact with our endocrine and nervous systems. Some stimulate the adrenal glands, others block hormone breakdown, and a few act like mild stimulants. The result? Blood vessels constrict, heart rate climbs, and blood pressure rises.
Top Herbs Known to Raise Blood Pressure
Below is a quick rundown of the most common culprits. Each has solid clinical or ethnobotanical evidence linking it to higher systolic or diastolic readings.
| Herb | Active compound(s) | Typical dose (adult) | Blood‑pressure effect | Key cautions |
|---|---|---|---|---|
| Licorice (Glycyrrhiza glabra) | Glycyrrhizin | 2‑5 g dried root daily | ↑ systolic by 5‑15 mmHg | Can cause hypokalemia, edema |
| Ephedra (Ma Huang) | Ephedrine, pseudo‑ephedrine | 0.5‑2 g dried herb | ↑ systolic by 10‑20 mmHg | Risk of arrhythmia, banned in many countries |
| Ginseng (Panax ginseng) | Ginsenosides | 200‑400 mg extract | ↑ systolic by 3‑8 mmHg | May interact with anticoagulants |
| Yohimbine (Pausinystalia johimbe) | Yohimbine alkaloid | 5‑20 mg per day | ↑ systolic by 5‑12 mmHg | Can cause anxiety, tachycardia |
| Cinnamon (Cinnamomum verum) | Cinnamaldehyde | 1‑6 g powdered | ↑ systolic modestly (2‑5 mmHg) | High doses may affect liver enzymes |
| Caffeine (Coffee, tea, guarana) | Caffeine | 200‑400 mg (≈2‑3 cups coffee) | ↑ systolic by 4‑8 mmHg | Can cause insomnia, jitteriness |
| Guarana (Paullinia cupana) | Guaranine (caffeine‑like) | 200‑500 mg extract | ↑ systolic by 3‑7 mmHg | Similar to caffeine side‑effects |
| Black Cohosh (Cimicifuga racemosa) | Isoflavones | 20‑40 mg extract | Potential slight rise, data limited | May affect hormone‑sensitive conditions |
How These Herbs Work: The Physiology Behind the Rise
Ephedra contains ephedrine, which mimics adrenaline. It binds to α‑ and β‑adrenergic receptors, causing vasoconstriction and a faster heart beat. Licorice’s glycyrrhizin blocks the enzyme 11β‑HSD2, leading to excess cortisol that acts like aldosterone-retaining sodium and water, which pushes up blood volume.
Ginseng’s ginsenosides have a mild stimulatory effect on the sympathetic nervous system, while yohimbine blocks α‑2 receptors, removing a natural brake on norepinephrine release. Even caffeine, though not an herb, is often present in herbal energy blends and works by antagonizing adenosine, which indirectly raises catecholamine levels.
Who Should Watch Their Intake
- People with diagnosed hypertension or pre‑hypertension.
- Those on antihypertensive medication (beta‑blockers, ACE inhibitors, diuretics).
- Pregnant or nursing mothers-some compounds cross the placenta.
- Individuals with kidney disease or heart rhythm disorders.
If any of these apply, treat herbal supplements like any other drug: check with a healthcare professional before adding them to your regimen.
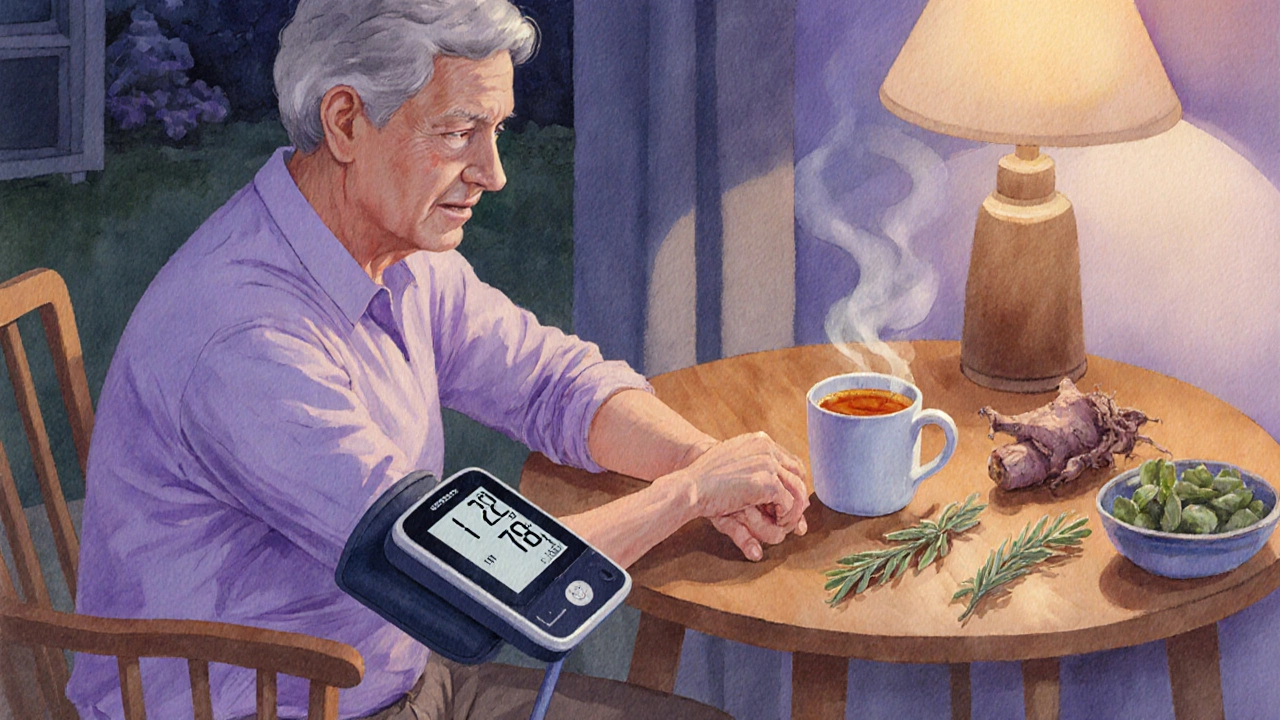
Safe Use Tips & How to Monitor Effects
- Start with the lowest possible dose. Many herbs have a dose‑response curve that plateaus after a certain point.
- Track your blood pressure daily for two weeks after starting an herb. Use a validated automatic cuff and log the numbers.
- Watch for ancillary signs: swelling in ankles, frequent urination, persistent headaches, or a rapid heartbeat.
- If you notice a consistent rise of 5 mmHg or more, discontinue the herb and discuss alternatives with a clinician.
- Prefer standardized extracts over raw powders when possible; they provide known amounts of the active compound.
Alternatives for Those Who Need a Boost Without the Pressure Spike
If you’re looking for energy, focus, or stress relief, consider herbs that are neutral or even modestly lower blood pressure. Adaptogens like Maca (Lepidium meyenii) or Rhodiola rosea generally don’t affect systolic values and have a good safety profile.
For mild blood‑pressure support, herbs such as hibiscus tea, garlic capsules, or omega‑3 enriched seeds can be beneficial without the risk of spikes.
When to Seek Professional Help
Any unexpected rise in blood pressure-especially accompanied by chest pain, shortness of breath, or visual disturbances-warrants immediate medical attention. Even if you think the herb is the culprit, a doctor can rule out other serious causes.
Bottom Line
Herbs can be powerful allies, but a handful of them-herbs increase blood pressure-are also capable of turning a healthy reading into a risky one. Knowing which plants to watch, how they act, and how to monitor their impact lets you enjoy nature’s pharmacy without endangering your heart.
Can licorice cause hypertension?
Yes. Licorice’s glycyrrhizin interferes with cortisol metabolism, leading to sodium retention and a rise in blood pressure, especially when consumed daily for more than a few weeks.
Is ephedra legal to use in supplements?
In many countries, including the United States and the European Union, ephedra is banned in dietary supplements due to safety concerns. Some Asian markets still allow limited use under strict dosage limits.
How quickly does caffeine raise blood pressure?
Caffeine peaks in the bloodstream within 30‑60 minutes, and systolic pressure can rise by 4‑8 mmHg during that window. The effect usually fades after 3‑5 hours.
Are there safe doses of yohimbine for blood‑pressure‑sensitive people?
Yohimbine is generally not recommended for anyone with hypertension. Even low doses (5 mg) can trigger a noticeable rise, so most clinicians advise avoiding it altogether.
Can I combine herbs that raise blood pressure with antihypertensive drugs?
Combining them can blunt the drug’s effect, leading to uncontrolled hypertension. Always discuss any herbal supplement with your prescribing physician.
