Hardest Mental Illnesses Explorer
Select a mental illness below to learn about its key characteristics, symptoms, and treatment options.
Schizophrenia
Chronic brain disorder with hallucinations and delusions
Bipolar Disorder
Extreme mood swings between mania and depression
Severe Depression
Persistent sadness and functional impairment
Borderline PD
Emotional instability and fear of abandonment
OCD
Intrusive thoughts and compulsive behaviors
DID
Multiple distinct personalities due to trauma
Condition Details
Select a condition above to view details.
Everyone hopes for a smooth mental life, but some conditions turn daily living into a constant battle. If you’ve ever wondered which diagnoses push the limits of coping, you’re in the right place. Below we unpack the illnesses that research, clinicians and lived‑experience accounts agree are the most debilitating, explain why they feel so hard, and give practical pointers for getting real help.
Understanding What Makes a Mental Illness Hard to Live With
Severity isn’t just about how “crazy” a label sounds. Clinicians use functional‑impairment scales - like the Global Assessment of Functioning (GAF) - to rate how much a disorder limits work, relationships and self‑care. The illnesses we’ll discuss typically score below 50, meaning they cripple everyday tasks. Common threads include chronic psychosis, extreme mood swings, pervasive anxiety that hijacks decision‑making, and symptoms that resist standard medication.
Schizophrenia - The Reality of a Fragmented Mind
Schizophrenia is a chronic brain disorder affecting about 1% of the global population, usually appearing in early adulthood, characterized by hallucinations, delusions, and disorganized thinking. The condition often forces people into isolation because reality feels unreliable. Auditory hallucinations can run nonstop, while delusional beliefs make trusting others nearly impossible. Even with antipsychotic medication, up to 30% of patients experience persistent negative symptoms - flat affect, social withdrawal, and reduced motivation - that erode quality of life.
Key challenges include:
- Difficulty distinguishing imagined from real experiences.
- Impaired executive function, making simple chores feel overwhelming.
- Social stigma that reduces employment opportunities.
Early intervention programs that combine low‑dose medication, cognitive‑behavioral therapy (CBT) and supported employment have shown the best outcomes, but continuity of care remains a hurdle.
Bipolar Disorder (Type I) - Riding Extreme Mood Swings
Bipolar Disorder (Type I) is a mood disorder marked by at least one full manic episode, often followed by depressive periods, affecting roughly 1.5% of adults worldwide. Manic phases can propel a person into risky behavior - overspending, impulsive driving, or hyper‑productivity that crashes into exhaustion. Depressive episodes then plunge them into hopelessness, sometimes with suicidal thoughts. The rapid cycling between highs and lows leaves families and employers guessing what the person will be like day‑to‑day.
Hard‑to‑manage aspects:
- Medication non‑adherence during mania, because the person feels “fine”.
- Sleep disruption - a core trigger for both poles.
- Co‑occurring anxiety or substance abuse, which magnifies instability.
Stabilizers such as lithium or atypical antipsychotics work best when paired with regular mood‑tracking and psychoeducation. Long‑term therapist support helps spot early warning signs before a full swing.
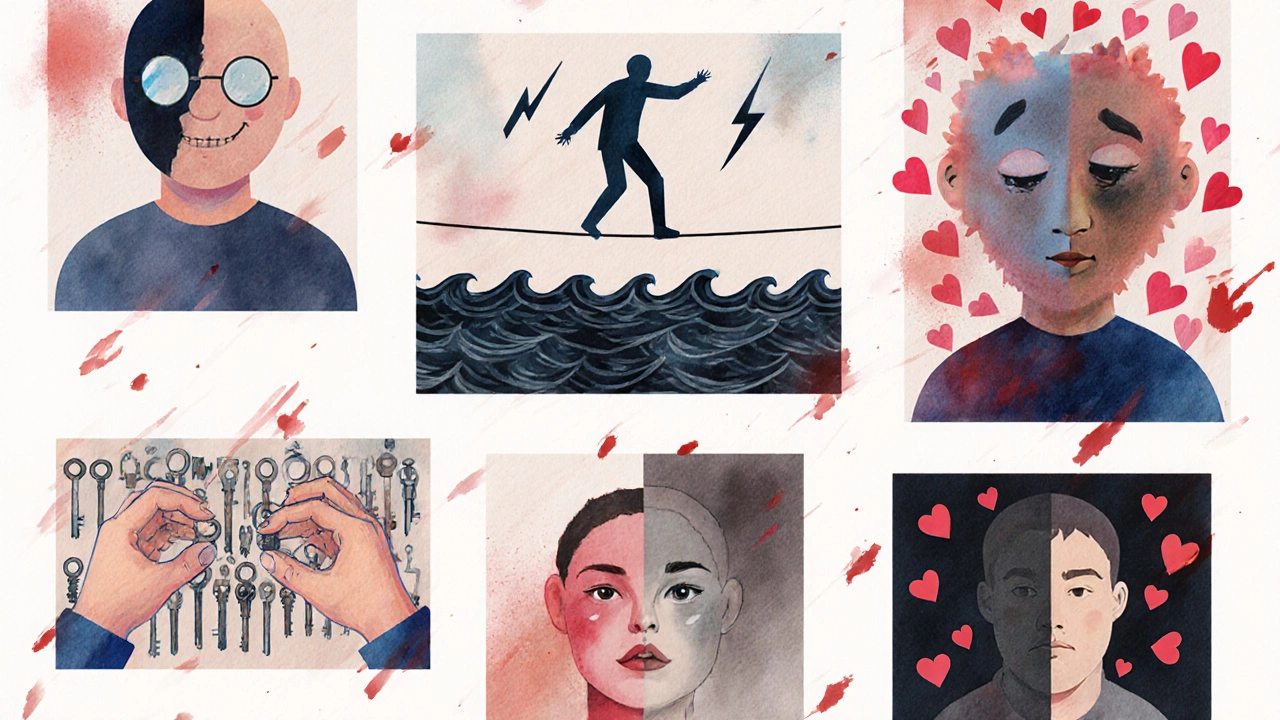
Severe Major Depressive Disorder - When Darkness Overwhelms
Severe Major Depressive Disorder is a mood disorder defined by persistent depressive mood, loss of interest, and functional impairment for at least two weeks, affecting about 7% of the population annually. In its worst form, the mind drags you into a vortex where even getting out of bed feels impossible. Cognitive speed slows, appetite falters, and thoughts of self‑harm become common. Unlike mild depression, severe cases often require combination therapy - antidepressants, psychotherapy, and sometimes electroconvulsive therapy (ECT).
Why it feels especially harsh:
- Psychomotor retardation - simple tasks take hours.
- Feelings of guilt that are disproportionate to reality.
- High suicide risk; the window for intervention can be narrow.
Rapid‑acting treatments like ketamine infusions have emerged as a lifeline for people who don’t respond to first‑line meds, but they need to be administered in specialist centres.
Borderline Personality Disorder - Emotional Instability on Steroids
Borderline Personality Disorder is a personality disorder characterised by intense fear of abandonment, unstable relationships, impulsivity and chronic feelings of emptiness, affecting roughly 2% of adults globally. The disorder’s hallmark is rapid mood shifts triggered by perceived slights. A simple comment can explode into rage, self‑harm, or frantic attempts to reconnect. These swings happen many times a day, making personal and work life feel like a roller coaster.
Components that make daily living tough:
- Emotional dysregulation - feelings feel 10× louder.
- Impulsive actions such as binge eating or reckless spending.
- Chronic sense of emptiness that fuels self‑destructive behaviours.
Dialectical Behaviour Therapy (DBT) is the gold‑standard, teaching skills to pause, label emotions, and build healthier coping mechanisms. Consistent therapy attendance is crucial because progress is measured in small, incremental gains.
Obsessive‑Compulsive Disorder - The Trap of Intrusive Compulsions
Obsessive‑Compulsive Disorder is an anxiety disorder marked by unwanted, persistent thoughts (obsessions) and repetitive behaviours (compulsions) performed to alleviate anxiety, affecting about 2-3% of adults worldwide. For many, the compulsions are time‑consuming rituals - checking doors 30 times, washing hands for hours, or arranging objects in a precise order. The anxiety that drives these rituals spikes the moment the routine is interrupted, creating a vicious cycle.
Why it feels unbearable:
- Hours lost each day performing rituals.
- Self‑criticism for being “irrational”, worsening anxiety.
- Social embarrassment that leads to isolation.
Exposure and Response Prevention (ERP) - a form of CBT - is the most effective therapy, gradually exposing the person to triggers while preventing the compulsive response. Some severe cases also need high‑dose SSRIs.
Dissociative Identity Disorder - Living with Multiple Selves
Dissociative Identity Disorder is a complex trauma‑related condition where two or more distinct personality states control behaviour alternately, affecting roughly 1% of the population, often under‑diagnosed. People report “switching” between identities that have different memories, preferences, and even physiological responses. Daily life can feel like sharing a body with strangers, leading to gaps in employment history, legal troubles, and fractured relationships.
Key hardships:
- Amnesia for events that occurred while another identity was present.
- Difficulty maintaining consistent treatment because different identities may have opposing views on therapy.
- High comorbidity with self‑harm and substance abuse.
Long‑term phase‑oriented trauma therapy, combined with a stable medication regimen for mood‑stabilisation, offers the best chance for integration of identities.

Post‑Traumatic Stress Disorder (Severe) - Constant Re‑lived Trauma
Severe Post‑Traumatic Stress Disorder is a disorder that develops after exposure to life‑threatening events, characterised by intrusive memories, hyperarousal and avoidance, affecting roughly 3-4% of adults globally. Flashbacks can feel as vivid as the original event, triggering a fight‑or‑flight response at the slightest reminder. Sleep is fragmented, and concentration suffers, making work or school almost impossible.
Factors that raise the burden:
- Nightmares that lead to chronic insomnia.
- Hypervigilance - constant scanning for danger.
- Avoidance of places or people linked to the trauma, limiting life experiences.
Evidence‑based treatments such as Trauma‑Focused CBT and Eye Movement Desensitization and Reprocessing (EMDR) reduce symptom intensity for many, but therapy length can span years, especially when co‑occurring depression is present.
How to Find Support and When to Seek Professional Help
No matter which condition you or a loved one faces, early engagement with mental‑health services can dramatically improve outcomes. Look for a psychiatrist or clinical psychologist who has experience treating severe cases; ask about their approach to medication management, psychotherapy type, and crisis planning.
Practical steps:
- Document symptoms daily - note triggers, duration, and intensity.
- Reach out to a trusted family member or friend for a supportive ear.
- Contact local mental‑health helplines (in India, the 080‑4611‑1111 “Snehi” helpline is free and confidential).
- If thoughts of self‑harm appear, go to the nearest emergency department or call emergency services (112 in India).
- Explore peer‑support groups - many run online via platforms like 7 Cups or local NGOs.
Remember, asking for help is a sign of strength, not weakness.
Quick Checklist for Managing Severe Mental Illness
- Stay on prescribed medication; set phone reminders.
- Schedule weekly therapy or support‑group sessions.
- Keep a simple routine - meals, sleep, light exercise.
- Identify early‑warning signs and have a crisis‑action plan.
- Limit substance use; it can exacerbate symptoms.
- Reach out for social connection, even when you feel withdrawn.
| Illness | Typical Onset Age | Key Impairments | Treatment Response |
|---|---|---|---|
| Schizophrenia | Late teens‑early 30s | Hallucinations, disorganized thought, social withdrawal | Partial; antipsychotics + psychosocial rehab |
| Bipolar Disorder (Type I) | 20‑40 years | Manic risk‑taking, depressive shutdown, sleep loss | Good with mood stabilizers + CBT |
| Severe Major Depressive Disorder | Any adult age | Psychomotor retardation, hopelessness, suicidality | Variable; antidepressants + therapy, sometimes ECT |
| Borderline Personality Disorder | Adolescence‑early adulthood | Emotional volatility, self‑harm, relationship storms | Improves with DBT; long‑term commitment |
| Obsessive‑Compulsive Disorder | Late childhood‑early adulthood | Time‑consuming rituals, anxiety, social avoidance | Responsive to ERP + high‑dose SSRIs |
| Dissociative Identity Disorder | Childhood (trauma) | Identity switches, memory gaps, self‑harm | Phase‑oriented trauma therapy + meds |
| Severe Post‑Traumatic Stress Disorder | After trauma (any age) | Flashbacks, hypervigilance, avoidance | Effective with TF‑CBT or EMDR; may need meds |
Frequently Asked Questions
What makes a mental illness “hard” compared to others?
Hardness is measured by functional impairment, chronicity, resistance to treatment and the degree to which symptoms dominate daily life. Disorders that cause psychosis, extreme mood swings or pervasive intrusive thoughts usually rank highest.
Can someone recover fully from these severe illnesses?
Full recovery - meaning no symptoms at all - is rare, but many people achieve substantial remission and lead productive lives with ongoing treatment, therapy and strong support networks.
Is medication always required?
Most of the illnesses listed benefit from medication to stabilize brain chemistry. However, the dosage, type and duration vary, and psychotherapy often plays an equally critical role.
How can families support a loved one with a severe mental illness?
Stay informed, encourage treatment adherence, create a low‑stress environment, and set clear boundaries. Joining caregiver support groups can also reduce burnout.
Where can I find affordable mental‑health care in India?
Government hospitals, NGO clinics (e.g., NIMHANS outreach), and tele‑psychiatry platforms like Practo or 1mg often provide low‑cost consultations. Many states also run free helplines for crisis support.
