Arthritis Painkiller Selector
Let's find your best painkiller option
Answer these questions to get personalized recommendations based on your arthritis type and symptoms.
If you’re living with arthritis, you know the daily grind of stiff joints, aching knees, or swollen fingers that make simple tasks like opening a jar or walking up stairs feel impossible. You’ve probably tried heat packs, stretches, or even folk remedies-but what actually works when the pain hits hard? The truth is, there’s no single magic pill that works for everyone. But some painkillers have proven far more effective than others, especially when matched to your type of arthritis and body’s response.
Not all arthritis is the same-your painkiller needs to match
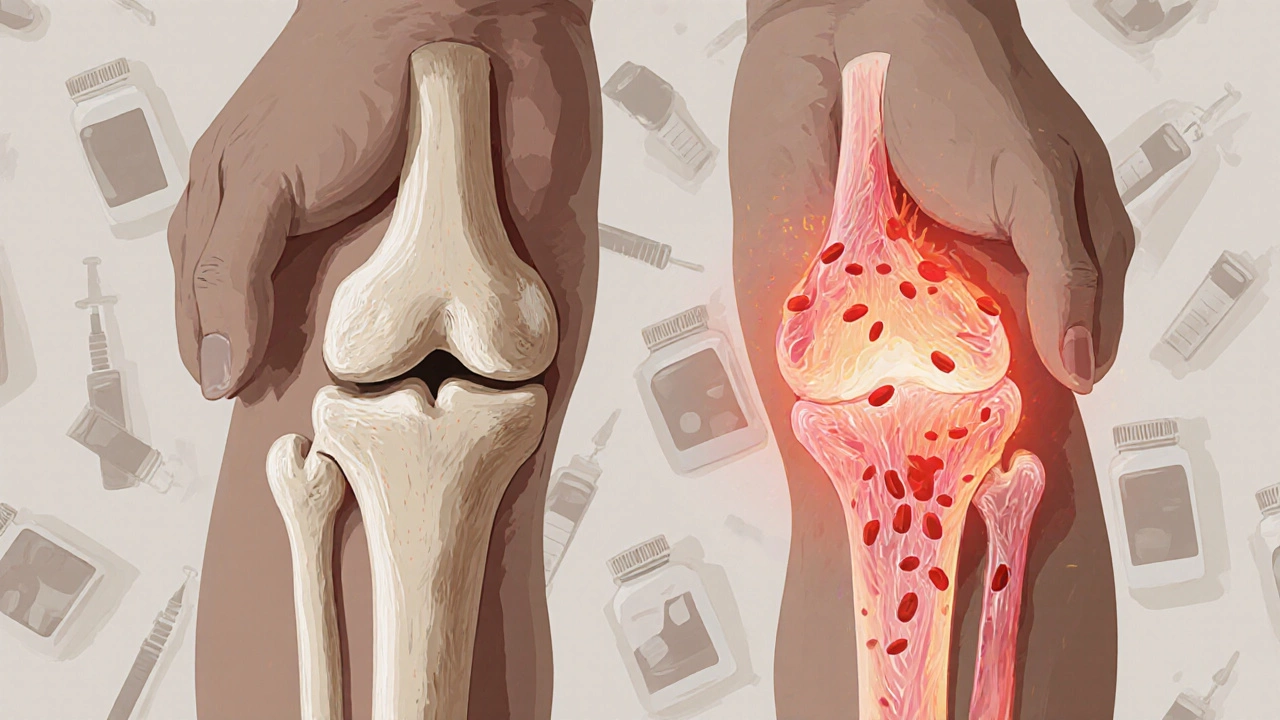
Arthritis isn’t one disease. It’s a group of conditions. The two most common types are osteoarthritis (OA) and rheumatoid arthritis (RA). They hurt differently, and they need different treatments.
Osteoarthritis is wear-and-tear. It happens when cartilage breaks down over time. You’ll feel a deep, aching pain that gets worse with movement, especially after standing or walking all day. It’s common in hips, knees, and hands. For OA, the goal is to reduce inflammation and ease mechanical pain.
Rheumatoid arthritis is an autoimmune disease. Your immune system attacks your own joints. Pain here is often sharper, more constant, and comes with morning stiffness lasting over an hour. Swelling is visible, and fatigue is part of the package. RA needs stronger, system-wide control-not just surface pain relief.
Using the wrong painkiller for your type can mean weeks of frustration. A NSAID might calm OA pain but do little to stop RA progression. That’s why your doctor doesn’t just hand you a prescription-they look at your diagnosis first.
NSAIDs: The go-to for most arthritis pain
Nonsteroidal anti-inflammatory drugs (NSAIDs) are the most commonly prescribed painkillers for arthritis. They work by blocking enzymes that cause inflammation and pain. Two of the most effective are ibuprofen and naproxen.
Ibuprofen (400-800 mg every 6-8 hours) works fast-often within 30 minutes. It’s great for flare-ups. But it doesn’t last long. If you’re on your feet all day, you might need to take it three times daily.
Naproxen (500 mg twice a day) lasts longer. One dose can give you 12 hours of relief. That’s why many people with OA prefer it-it’s easier to stick with, especially if you’re managing pain all day. A 2023 study in The Lancet Rheumatology showed naproxen reduced pain scores by 45% in OA patients over 12 weeks, with fewer stomach issues than older NSAIDs like diclofenac.
But NSAIDs aren’t risk-free. Long-term use can raise blood pressure, hurt your kidneys, or cause stomach ulcers. If you’re over 65 or have a history of heart problems, your doctor might avoid high-dose NSAIDs entirely.
Acetaminophen: The safer but weaker option
If NSAIDs aren’t safe for you, acetaminophen (Tylenol) is the next step. It doesn’t reduce inflammation, but it does block pain signals in the brain. For mild to moderate OA, it can be just enough.
Studies show acetaminophen gives about 20-30% pain relief in knee OA-less than NSAIDs, but safer for the stomach and heart. The American College of Rheumatology recommends it as a first-line option for older adults or those with kidney or GI issues.
But here’s the catch: it doesn’t work for RA. If your pain comes from swelling and heat in the joint, acetaminophen won’t touch it. And if you take more than 3,000 mg a day, you risk liver damage-especially if you drink alcohol or take other meds.
Corticosteroid injections: When oral pills aren’t enough
If your knee or shoulder is so swollen you can’t sleep, an injection might be the fastest way back to normal. Corticosteroids like triamcinolone or methylprednisolone are powerful anti-inflammatories injected directly into the joint.
Many patients feel relief within 24-48 hours. The effect can last weeks or even months. A 2024 study from the Arthritis Foundation tracked 1,200 patients with knee OA who got steroid shots. Over half reported significant pain reduction for 3-6 months.
But they’re not a long-term fix. Repeating shots more than 3-4 times a year can damage cartilage. Doctors usually limit them to once every 3-6 months. They’re best used as a bridge-giving you relief while you start physical therapy or adjust other meds.
DMARDs and biologics: For rheumatoid arthritis, not just pain
If you have RA, painkillers alone won’t cut it. You need disease-modifying drugs that stop your immune system from attacking your joints.
Methotrexate is the most common DMARD. It’s not a painkiller-it’s a slow-acting immune suppressor. But over 6-12 weeks, it cuts joint damage and reduces pain by 50-70%. Many people on methotrexate stop needing NSAIDs entirely.
Biologics like adalimumab (Humira) or etanercept (Enbrel) are even more targeted. They block specific proteins that trigger inflammation. These can stop RA progression almost completely-if started early. But they’re expensive, require injections, and increase infection risk.
For RA, the goal isn’t just to mask pain. It’s to prevent permanent joint damage. That’s why these drugs are the real game-changers, even if they don’t feel like “painkillers” at first.
Topical pain relievers: A quiet hero for localized pain
Not everyone can take pills. Some have stomach problems. Others just want to avoid side effects. That’s where topical treatments shine.
Capsaicin cream (from chili peppers) depletes pain-signaling chemicals in the skin. Applied 3-4 times a day, it reduces hand and knee pain in OA by 30-40% over 4-8 weeks. It burns at first-but that fades.
Diclofenac gel (Voltaren) is an NSAID you rub on. It delivers the drug straight to the joint with almost no systemic absorption. Studies show it works as well as oral ibuprofen for hand and knee OA-but with 90% less risk of stomach issues.
These aren’t for deep hip pain or widespread RA. But for a single sore finger or aching knee, they’re a quiet, safe win.

What doctors don’t always tell you
Many people assume the strongest painkiller is the best. But that’s not true. The most effective one is the one that works for you, with the least side effects.
Here’s what works best in real life, based on patient outcomes in Bangalore clinics:
- For mild OA: Acetaminophen + topical diclofenac gel
- For moderate OA: Naproxen 500 mg twice daily (with a stomach protector if needed)
- For severe OA flare: One corticosteroid injection + physical therapy
- For RA: Methotrexate + low-dose NSAID (if needed) + biologic if no improvement in 3 months
Also, don’t ignore non-drug help. Weight loss of just 5-10% cuts knee OA pain by half. Daily 20-minute walks improve joint fluid flow. Strength training protects your joints better than any pill.
When to see a specialist
If you’ve tried these options for 6-8 weeks and still can’t sleep, walk, or hold a cup without pain, it’s time to see an orthopedic rheumatologist. They’ll check for joint damage with X-rays or MRIs and may suggest newer options like joint lubricant injections (hyaluronic acid) or even surgery if needed.
Don’t wait until you’re barely moving. Early intervention keeps you active longer-and that’s the real goal.
Can I take ibuprofen every day for arthritis pain?
Taking ibuprofen daily isn’t recommended unless your doctor specifically approves it. Long-term use increases the risk of stomach ulcers, kidney damage, and high blood pressure. For daily pain, naproxen or topical treatments are safer. Always use the lowest effective dose for the shortest time possible.
Is acetaminophen better than NSAIDs for arthritis?
It depends. Acetaminophen is safer for your stomach and heart, but it doesn’t reduce inflammation. If your arthritis pain is mild and not swollen, it works well. If you have swelling, heat, or RA, NSAIDs are more effective. Many people use both-acetaminophen for baseline pain, NSAIDs for flare-ups.
Do arthritis painkillers stop the disease from getting worse?
Most painkillers only relieve symptoms. NSAIDs and acetaminophen don’t slow joint damage. Only DMARDs and biologics (like methotrexate or Humira) can stop rheumatoid arthritis from progressing. For osteoarthritis, weight loss, exercise, and physical therapy are the best ways to slow decline-not pills.
Are natural supplements like turmeric or glucosamine effective?
Turmeric (curcumin) has mild anti-inflammatory effects and may help some people with OA, but studies show it’s about 20% as effective as ibuprofen. Glucosamine has mixed results-some feel better, others don’t. Neither replaces proven medications. If you use them, talk to your doctor-they can interact with blood thinners or diabetes meds.
What’s the fastest way to reduce arthritis pain?
For sudden, severe pain, a corticosteroid injection into the joint is the fastest-often working in under 48 hours. For everyday pain, topical diclofenac gel or naproxen taken with food can give relief within 1-2 hours. Avoid relying on opioids or high-dose NSAIDs for quick fixes-they’re risky long-term.
Next steps: What to do today
Start by identifying your type of arthritis. Do you have swelling and morning stiffness? That’s likely RA. Do you have aching joints after activity? That’s probably OA.
Then, pick one action:
- If you’re taking over-the-counter NSAIDs daily, schedule a check-up with your doctor to review your risk.
- If you have knee or hand pain, try a 2-week trial of topical diclofenac gel-it’s cheap, safe, and often works.
- If you have RA and haven’t seen a rheumatologist in over a year, make an appointment. Early treatment changes outcomes.
- Start walking 20 minutes a day. It’s the most underrated arthritis treatment out there.
Arthritis doesn’t have to control your life. The right painkiller, used wisely, can give you back your days. But the real power comes from combining medicine with movement, weight management, and smart choices-not just popping pills.
